Mouth Breathing: Why it Matters and How Myofunctional Therapy can help
May 2023 | Samantha Lovegreen, M.S. CCC-SLP
How can myofunctional therapy improve your child’s quality of sleep, speech, and overall oral wellness?
This blog will focus on:
What is Mouth Breathing and what are the benefits of nasal breathing?
How Mouth Breathing affects oral function?
How Mouth Breathing impacts sleep?
How Myofunctional Therapy can help?
Who to refer to?
Often parents bring their child into our clinic with concerns such as others cannot understand their child or that their child has persistent speech sound errors. As any speech-language pathologist would I immediately start thinking about; what types of speech sound errors are, whether are they using any phonological processes, and how to improve intelligibility. But I have also learned how important it is to pay close attention to a child’s mouth and facial movements. So here is when I start to wonder where the tongue and mouth muscles are when the child’s mouth is at rest, drinking, eating, and speaking.
At this point in the evaluation process, I start to ask further questions like, “Does your child breath through his/her mouth or nose?”, “Does your child have any trouble sleeping?”, “Does he/she get sick often?”, and “Did he/she have any difficultly when breastfeeding?”. These questions at first seem unrelated to the parent’s current speech concerns; however, are essential in making an accurate diagnosis. When parents start to answer these questions, I often find out their child is a mouth breather and speech sound errors are just one piece of the puzzle. Through completion of coursework in Orofacial Myofunctional Therapy, I have learned how mouth breathing impacts a child and the role a Speech Language Pathologist has in treating it!
What is mouth breathing?
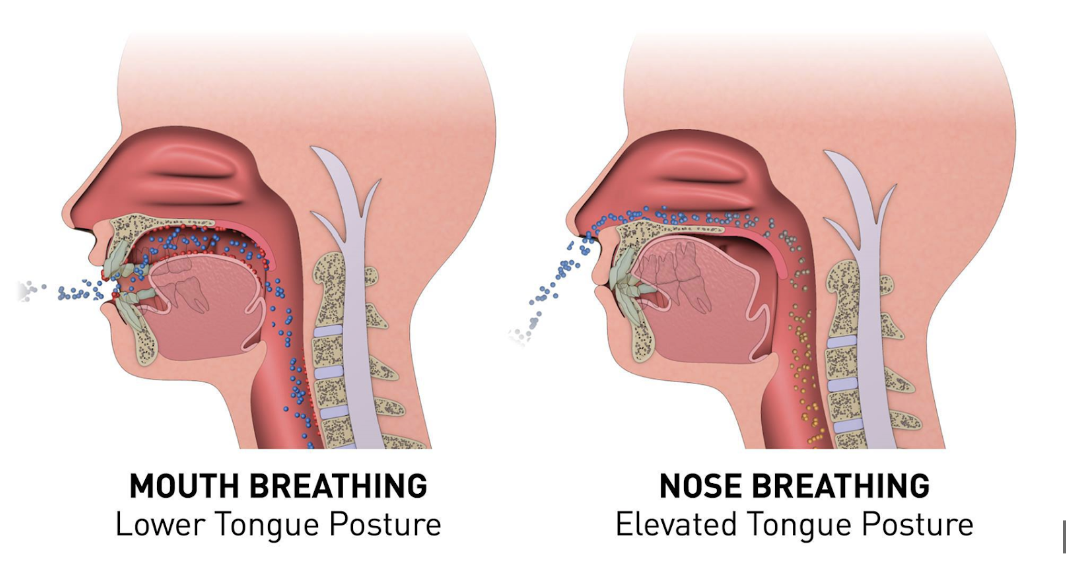
Mouth Breathing is when an individual breathes primarily through their mouth. According to the ASHA leader, mouth breathing is seen in 55% of children. The biggest difference between mouth and nasal breathing is filtration. Nasal breathing helps to filter out foreign particles from the surrounding environment and therefore helps deliver air with less contaminants to the respiratory system. When breathing through your mouth the air is not filtered before it reaches the lungs. There is an increased likelihood of colds, infections in the nose/throat, and chronic ear infections in children who mouth breathe. Potential causes of mouth breathing include; problems with mouth and bite structure, enlarged tonsils and adenoids, nasal congestion due to allergies, and deviated septum.
Signs of Mouth breathing in children:
Chronic fatigue
Hoarseness
Bad Breath
Dry/cracked lips
Irritability
Consequences of Mouth Breathing include:
Underdeveloped Jaw
Lip incompetence
Crocked/overcrowding teeth
Narrow facial features
Hyperactivity and impulsivity
Frequent awakening at night
Daytime sleepiness
Increased behavioral problems
Mouth breathing also modifies how a child’s mouth functions across a variety of tasks including; resting, chewing/swallowing, and speaking.
Oral Rest Posture: Mouth breathing causes a child to have an open-mouth oral rest posture with noticeable open lips and low tongue position. This can result in excess saliva and drooling when the mouth is at rest.
Chewing/Swallowing: Mouth breathing can cause a child to chew food with their lips apart, which can be noisier and less productive than chewing with lips closed. This can also result in digestive issues and potential choking when a child has difficulty coordinating when/how to breathe when their mouth is full of food. When swallowing, a child may protrude their tongue through their front teeth and/or compensate with tension in the muscles around the mouth or increased head movements. Mouth breathers may have reduced strength for chewing and swallowing and therefore prefer softer foods and/or use liquid to help when swallowing.
Speech: Distortions of speech sounds may also be present such as tongue protrusion between the teeth when making an /s/ and /z/ or low tongue placement when producing sounds such as /t, d, n, l/.
What about mouth breathing at night?
Daytime mouth breathing patterns are often seen when a child is sleeping, during which time the muscles of the mouth and face are relaxed. Mouth breathing can be the root of sleep-disordered breathing. Sleep-disordered breathing is any abnormal breathing patterns during sleep.
Mouth breathing at night can cause many symptoms including:
Restless sleep
Snoring
Headaches
Drooling on the pillow
Thirst when waking up
Morning sleepiness
Sleep apnea (breathing interruptions during sleep)
Decreased oxygen saturation in the blood.
In summary, the ASHA leader describes “the ability to breathe effortlessly and quietly through the nose with the tongue suctioned up and the lips gently closed is essential to optimal craniofacial growth and development. Healthy nasal breathing supports proper oral functions (including oral resting posture, swallowing patterns, chewing, and speaking), voicing, and overall body posture. When nasal breathing goes awry, orofacial myofunctional disorders may result, raising red flags to clinicians.”
How Myofunctional therapy can help?
SLPs with proper training in orofacial myofunctional therapy, as part of an interdisciplinary team, can be essential in providing treatment for abnormal breathing patterns and oral functions.
The interdisciplinary team may include:
ENTs
Allergists
Airway-centric pediatric dentists and orthodontists
Physical and occupational therapists
Myofunctional therapy can work to establish an appropriate oral rest posture. In the correct oral rest posture; the tongue should be resting at the roof of your mouth, the teeth should be gently closed, and lips should close. A variety of exercises can be implemented to address nasal breathing, lip closure, and tongue suctioning to the palate. In addition, treatment can work on correct placement of the tongue and lips while chewing/swallowing and producing speech sounds.
SLPs can also help children and families develop healthy sleep patterns including:
Establish and maintain nightly bedtime routines, attempting to keep bedtime consistent Monday –Sunday to promote a natural sleep-wake cycle.
Turn down the lights to prepare the body for sleep and put electronics and screens away, at least one hour before bedtime.
Unwind the mind and body through simple yoga poses, breathing exercises, and/or mediation
For further information, check out the following websites:
Academy of Orofacial Myofunctional Therapy. 2022. Frequently asked questions, related to Mouth Breathing https://aomtinfo.org/faq/
American Speech-Language-Hearing Association. 2022. Orofacial Myofunctional Disorders. https://www.asha.org/practice-portal/clinical-topics/orofacial-myofunctional-disorders/#collapse_6.
References:
The ASHA Leader. 2018. Health Breathing, ‘Round the Clock.’ Problems with airway functioning during sleep can hurt children’s health. And SLPs, alongside other professionals, are on the front lines of identification and intervention. https://leader.pubs.asha.org/doi/10.1044/leader.ftr1.23022018.48